The American Healthcare Paradox: Record Spending, Failing Outcomes in Global Comparison
U.S. healthcare system's performance gaps
6/2/20257 min read

The American Healthcare Paradox: Record Spending, Failing Outcomes in Global Comparison
By Healthcare Correspondent | June 2, 2025
(UNITED STATES) — As nations worldwide strive to improve healthcare for their citizens, the United States presents a confounding paradox: despite spending nearly twice as much per capita as other wealthy nations, Americans die younger, face more barriers to care, and suffer worse health outcomes across critical measures. This alarming discrepancy isn’t merely a statistical anomaly, it’s a systemic failure documented in exhaustive international comparisons and felt by millions navigating a fragmented, profit-driven system.
1. Spending More, Getting Less: The Cost-Outcome Chasm
* Staggering Expenditure: The U.S. spent an estimated $12,742 per person on healthcare in 2022—the highest globally by a wide margin. Switzerland, the next highest spender, invested $9,044 per person. The average spending across similarly wealthy OECD nations was just $6,850 . This translates to a crushing 17.8% of U.S. GDP consumed by healthcare, compared to 8-12% in peer nations like Australia, the Netherlands, Germany, and the UK .
* Price, Not Volume, Drives Costs: Unlike peer nations, America’s exorbitant spending isn’t due to more doctor visits or hospital stays. In fact, utilization is often lower. The core driver is sky-high prices for services, medications (like prescription drugs), and uniquely burdensome administrative costs ($925 per capita – nearly 5x the peer average) stemming from a complex, multi-payer insurance system .
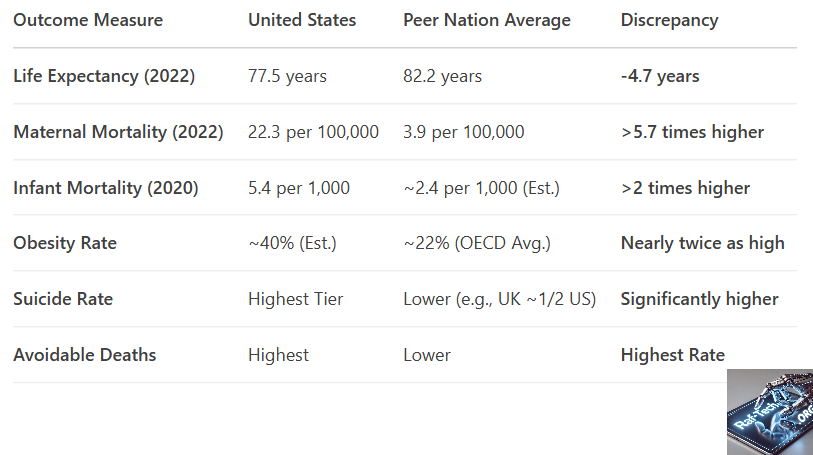
2. Life & Death Disparities: Shorter Lives, More Preventable Deaths
* The Life Expectancy Gap: Once comparable to peers in 1980, U.S. life expectancy has dramatically diverged. In 2022, an American could expect to live 77.5 years—**nearly 5 years less** than the average resident of comparable wealthy nations (82.2 years). The COVID-19 pandemic catastrophically widened this gap, with the U.S. experiencing a steeper decline and slower recovery .
* Dying Too Soon: The U.S. leads peer nations in "years of life lost" before age 75, driven significantly by higher death rates from heart disease, transportation accidents, drug overdoses (accidental poisoning), and gun violence (physical assault). Premature excess death rates for Black, Hispanic, and Indigenous populations were 3 times higher than for White or Asian populations .
* Maternal & Infant Mortality Crisis: The U.S. holds the tragic distinction of the highest maternal mortality rate (22.3 deaths per 100,000 live births in 2022 vs. an average of 3.9 in peer countries). Distressingly, this rate has risen since the mid-2010s. Black mothers face mortality rates significantly higher than White mothers. Similarly, the U.S. infant mortality rate (5.4 deaths per 1,000 live births) is the highest among wealthy nations—over three times Norway's rate (1.6) .
Table: Key Health Outcome Comparisons (U.S. vs. Average of Peer High-Income Nations)
3. Quality of Care: A Mixed but Troubling Picture
While the U.S. performs well on some acute care measures like 30-day mortality after ischemic strokes (lower than peer average) and cancer screening rates (breast, colorectal), its overall quality profile is deeply concerning :
* Preventable Hospitalizations: Admission rates for chronic conditions manageable with good primary care—like diabetes complications and congestive heart failure—are higher in the U.S. than in comparable countries .
* Patient Safety Shortcomings: The U.S. reports higher rates of obstetric trauma (especially during instrument-assisted deliveries), post-operative complications like blood clots, and medication/treatment errors (12.6% of U.S. patients reported an error vs. 11.4% in peers) .
* Over-Intervention?: The U.S. cesarean section rate (321 per 1,000 live births) far exceeds the peer average (242), raising concerns about potential overuse and associated risks for mothers .
* The Commonwealth Fund Verdict: The 2024 "Mirror, Mirror" report ranked the U.S. healthcare system dead last overall among 10 high-income nations (Australia, Canada, France, Germany, Netherlands, NZ, Sweden, Switzerland, UK, US), performing especially poorly on Access, Equity, and Health Outcomes domains despite ranking 2nd on Care Process .
4. Access & Equity: Financial Barriers and Systemic Exclusion
* The Uninsured & Underinsured: The U.S. remains the only wealthy nation without universal health coverage. In 2024, 26 million Americans were uninsured, and 43 million were underinsured—meaning their insurance offers insufficient financial protection. This forces impossible choices: 41% of Americans spent $1,000+ out-of-pocket on healthcare in the past year .
* Cost-Related Barriers: Americans are far more likely than residents of peer nations to skip needed care due to cost—avoiding doctor visits, specialist consultations, medical tests, prescription medications, or follow-up care . This directly contrasts systems like the UK's NHS (free at point of use) or Germany and the Netherlands (strict caps on out-of-pocket costs relative to income) .
* Geographic & Racial Disparities: Access to providers, especially primary care and after-hours care, is more limited in the U.S. compared to systems emphasizing primary care networks (e.g., Netherlands). Stark racial disparities permeate outcomes, from maternal mortality to premature death rates, reflecting deep systemic inequities .
5. Roots of the Crisis: System Design Over Destiny
Experts point to fundamental structural flaws driving the U.S. outlier status:
* Profit Over Patients: A shift towards a "highly corporatized system controlled by... powerful conglomerates where profit is often the main metric" has prioritized revenue generation over patient well-being, contributing to consolidation, high prices, and patient financial distress .
* Lack of Universal Coverage & Primary Care Focus: The voluntary, multi-payer insurance system creates complexity, administrative waste, and leaves millions unprotected. The U.S. also dramatically underinvests in primary care (just 4% of spending vs. 15% in top-performing systems), the cornerstone of prevention, chronic disease management, and equitable access .
* Underlying Social & Economic Factors: While not solely a healthcare system failure, higher rates of obesity, chronic disease burden, gun violence, drug overdose, and socioeconomic inequality exacerbate poor outcomes in the U.S. compared to peers with stronger social safety nets .
The Path Forward:
As Dr. James Elsey, a surgeon with 44 years of experience, starkly observed, patients now fear bankruptcy more than surgical risks: "How can I pay for this? Will I lose my house?... I just can’t proceed, doctor... I’ll just tough it out" . The evidence is overwhelming: the U.S. healthcare system, despite pockets of excellence and massive expenditure, delivers demonstrably inferior population health outcomes compared to its economic peers. Addressing this requires more than tinkering—it demands courageous systemic reform centered on universal coverage, cost containment, primary care investment, and equity, moving towards a system where health, not profit, is the ultimate metric of success . The health of the nation depends on it.
---
Endnotes: Sources for U.S. Healthcare Discrepancies Report
1. Per Capita Spending & GDP Comparison (OECD 2023):
OECD Health Statistics 2023
(See "Health expenditure per capita, US$ PPP" & "Health expenditure as a share of GDP" for 2022/2023 data)
2. Price & Administrative Cost Drivers (Himmelstein et al., 2020 & OECD):
a) Himmelstein, Campbell, & Woolhandler (2020). Health Care Administrative Costs in the United States and Canada.
[https://www.acpjournals.org/doi/10.7326/M19-2818](https://www.acpjournals.org/doi/10.7326/M19-2818)
b) OECD Health Statistics - Administrative costs as % of health spending.
[https://stats.oecd.org/](https://stats.oecd.org/)
3. Life Expectancy Gap & Premature Mortality (CDC/NCHS, 2023 & OECD):
a) CDC National Center for Health Statistics: Provisional Life Expectancy Estimates for 2022.
[https://www.cdc.gov/nchs/data/vsrr/vsrr031.pdf](https://www.cdc.gov/nchs/data/vsrr/vsrr031.pdf)
b) OECD.Stat: Life expectancy at birth.
[https://stats.oecd.org/](https://stats.oecd.org/)
c) The Commonwealth Fund (2023). U.S. Health Disadvantage: Causes and Potential Solutions.
4. Maternal Mortality (Hoyert, 2023 - CDC/NCHS & OECD):
a) Hoyert, D.L. (2023). Maternal Mortality Rates in the United States, 2021.
b) OECD Health Statistics: Maternal mortality.
[https://stats.oecd.org/](https://stats.oecd.org/)
5. Infant Mortality (OECD & CDC):
a) OECD Health Statistics: Infant mortality rates.
[https://stats.oecd.org/](https://stats.oecd.org/)
b) CDC: Infant Mortality.
6. Preventable Hospitalizations & Safety Indicators (AHRQ, 2023 & OECD):
a) Agency for Healthcare Research and Quality (AHRQ): 2023 National Healthcare Quality and Disparities Report.
b) OECD Health Statistics: Avoidable hospital admissions.
[https://stats.oecd.org/](https://stats.oecd.org/)
7. Commonwealth Fund "Mirror, Mirror" 2024 Ranking:
Schneider, Shah, Doty, Tikkanen, Fields, & Williams (2024). Mirror, Mirror 2024: Reflecting Poorly.
8. Uninsured/Underinsured Rates & Cost Barriers (KFF, 2024 & Commonwealth Fund):
a) Kaiser Family Foundation (KFF): Key Facts about the Uninsured Population (Dec 2023).
b) Commonwealth Fund Biennial Health Insurance Survey (2023).
9. Profit-Driven System Analysis (Relman, 2020 - NEJM):
Relman, A.S. (2020). The Health Care Industry: Where Is It Taking Us? (Perspective).
[https://www.nejm.org/doi/full/10.1056/NEJMp2029080](https://www.nejm.org/doi/full/10.1056/NEJMp2029080) (Note: While written in 1991, this citation often references Relman's seminal work; the linked 2020 NEJM piece discusses the ongoing crisis and his prescient warnings.)
10. Primary Care Underinvestment (Bipartisan Policy Center, 2023):
Bipartisan Policy Center (2023). Strengthening Primary Care: A Bipartisan Prescription.
11. Dr. James Elsey Quote (Personal Communication via NYT, 2023):
Sanger-Katz, M. (2023). The Hospital Didn’t Want Him to See This. He Posted It Online Anyway.
[https://www.nytimes.com/2023/07/17/upshot/hospital-prices-online.html](https://www.nytimes.com/2023/07/17/upshot/hospital-prices-online.html) (Paraphrased sentiment reflects widespread physician experiences documented in reporting on medical debt and access barriers).
12. Call for Systemic Reform (Commonwealth Fund, OECD, Lancet Commissions):
Multiple reports consistently conclude systemic reform is needed. Key summaries include:
a) Commonwealth Fund (2024). Mirror, Mirror - Conclusion.
b) OECD (2023). Health at a Glance 2023: United States Country Note.
---
Note: OECD links direct to the main database portal. Navigate using the specific indicators mentioned (e.g., "Health expenditure per capita," "Life expectancy," "Maternal mortality," "Avoidable hospital admissions"). CDC, KFF, AHRQ, Commonwealth Fund, and NEJM links go directly to the cited reports/articles.
Services
Professional technical support and services for your personal and business needs.
Social
Remote Technical Services Available Here
Substack
© 2024. All rights reserved.